Written By
Kevin Murray, M.A. (pending)
Movement Masterminds – CEO
Function First – Director of Education
2012 CSEP CPT of the Year
THE SIZING APPEAL
The Small, Medium, Large concept to clothing that all department stores embody seems like a straightforward, pragmatic approach to sizing. If the article of clothing fits, you’re golden; If not, you’re either going up a size, or down. But what about those that fall between the cracks? Or above, or below those labels?
I constantly run into this predicament. Sometimes a small is too tight. Other times a medium drapes off my shoulders, which was a good look for me in the 90’s with skateboard in hand – not so cool anymore. I often wish there was a size “smedium”, right in between at that “sweet spot.”
Perhaps you can relate… maybe your frame deserves a “marge”, right in between medium and large.
ATTENTION ALL “SHOPPERS”:
DUALISTIC THINKING IS OUT-OF-DATE & NO LONGER IN STOCK!
Am I really posting up an article about clothing? As much as I dig fashion, the department store approach is actually a metaphor for the movement industry in many respects, and its modus operandi to complex pain problems.
For example, you may be familiar with conceptualized strategies such as:
• Tight hips = stretch em’
• Weak glutes = strengthen em’
• Noticeable swelling = ice that sh#t
• IT Band irritation = foam roll those puppies
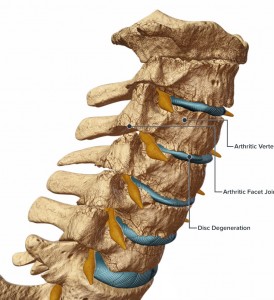
A dualistic, department store approach emphasizes that although all individual’s move differently and come from different backgrounds and cultures, there are essentially only 3-types of people – small, medium and large. Chronic pain on the other hand is complex, embodying dynamic dimensions that encompass myriad variables expanding beyond the optics of biomechanical and connective tissue principles alone. A diverse approach to sizing is needed.
GEORGE ENGEL’s BPS APPROACH:
TAILORED FOR ALL SHAPES AND SIZES – SINCE 1977
Progressing beyond (but not excluding) biomechanics and connective tissue, a 3-dimensional approach to working with clients’ in pain include a vast variety of biopsychosocial ingredients and considerations:
• Systems theories
• Empathetic listening
• Uncovering client’s’ values and beliefs systems
• Establishing client trust
• Providing educational dividends around the context of pain
• Explaining the protective purpose that pain serves
are all in play when considering the Neuromatrix and its influence on how we collaborate with, and coach our clients’ in pain.

SUIT YOU, SIR
Working with the chronic pain demographic is much like being a tailor. Each individual comes in with unique dimensions and constraints; different outcomes and desires. A tailor is seeking to understand where specific attention needs to be placed. A tailor asks questions like:
Why doesn’t their clothing fit?
Have they ever been to a tailor before? If so, what was their experience?
How will we know when a successful amendment has taken effect?
What is their specific outcome?
A tailor considers multiple dimensions into his/her analysis and thought process, outside the shackles of unidimensional constraints. Instead, diversification is personified, driven by the uniqueness of each individual and their articles of clothing.
Individuals’ in pain each have their own unique articles of clothing (yes, we’re still talking metaphorically here) that need specific attention and consideration. If you can meet your clients’ unique needs, much like a tailor does, than you’ll have accomplished something truly special in your clients’ eyes.
Amidst the waves of uncertainty that accompany working with individuals’ experiencing chronic pain and relinquishing a dualistic/department store thought-process, above all remember you’re interacting with another individual – and not a mechanistic instrument. Be kind, be empathetic, and as often as possible seek to understand rather than judge.
“The quality of the therapeutic relationship appears to be more predictive of success than any theoretical approach of the helper.” John Nuttall