Magnetic resonance imaging (MRI) is one of the most sensitive diagnostics currently available. It has frequently been the “last word” on pain, surgery and recommended limitations on activity. But should your client really never lunge or squat again because their doctor took an MRI and it showed some pathological condition?
Consider this review I did of a couple of studies on the matter. You may change the conversation you have with your clients once finished reading this.
Guermazi et. al. (2012) used magnetic resonance imaging to look at knees where radiographic imaging (x-rays) showed no osteoarthritic (OA) changes. OA is generally diagnosed through examination and x-ray. X-rays can identify bony changes to the joint but they cannot identify soft tissue pathologies. The purpose was to use the more sensitive MRI to detect structural lesions associated with OA and their relationship to age, sex and obesity.

710 subjects age 50 or older participated in the study (mean age 62.3 years). Out of the 710 subjects, 206 (29%) had painful knees.
Overall, 610 (89%) of the subjects showed some abnormality of the knee. Three most common findings of abnormalities in the knee were osteophytes, cartilage damage and bone marrow lesions. These abnormalities increased with age.
The study concluded that 91% of those who did have pain in their knee also had abnormal MRI’s, leaving 9% of those with painful knees having normal MRI’s. And 88% of those with no pain in their knees showed abnormalities in the MRI. The authors also noted that those with the highest amount of abnormalities in their MRI were those identified with mild pain and not those with moderate or severe pain (emphasis mine).
Another study in European Spine Journal (Kato et al. 2012) looked at MRI’s of the cervical spine of 1211 asymptomatic patients. The subjects were both men and women equally distributed between the ages of 20 years to 70 years. All of the subjects had both an MRI and neurological exam by a spinal surgeon.
Findings from the MRI of spinal cord compression, spinal cord signal changes and disc compression were noted. Increased signals on an MRI are associated with an abnormal state of the tissue such as scarring of inflammation.
For a disc bulge to be considered pathological it had to measure more than 1 millimeter from the vertebral body.
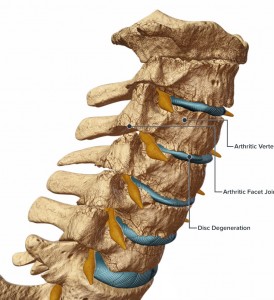
Of the 1211 asymptomatic subjects studied, 64 (5.3%) had spinal cord compression. High intensity signal changes were seen in 28 (2.3%) and disc bulging was seen in 1061 (87.6%) of subjects. Prevalence of these findings was significantly higher in people over 40 years of age.
If we consider the findings of both these studies, it is now clear that degenerative changes to the body are a normal part of aging and do not directly correlate with pain. Clients may experience stress or fear when learning of abnormalities in any joint or soft tissue following imaging studies done on them. Even if they are not in pain but have experienced pain in the past, the knowledge of degenerative changes are often communicated by medical professionals and perceived by individuals as the sole source of their pain. These studies clearly demonstrate that an individual can have many abnormal finding in the neck and knees and have no pain.
Clients who believe that the degenerative changes on their imaging will lead to pain may potentially act with self-limiting and guarded movements as well as an expectation of pain. This has the potential to decrease their functional capacity, increase anxiety about certain exercises or activities and view surgery as a necessary step to resolution.
Although I’ve suggested that your conversation should change with your clients, when you understand what these studies (and others) are telling us, we must remember that your client’s paradigm may not easily change. Their beliefs may be entrenched in an outdated pain/imaging relationship, especially if their doctor leads them to believe that the MRI finding is the final word.
They need proof. And ultimately that proof is movement confidence.
Guermazi, Ali August 2012. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ, 345:e5339 doi: 10.1136/bmj.e5339).
Kato, Fumihiko et al. February 2012. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: magnetic resonance imaging of over 1,200 asymptomatic subjects. Eur Spine J, DOI 10.1007/s00586-012-2176-4.
Tags: arthritis, knee pain, MRI, neck pain, osteoarthritis
PLEASE PLEASE PLEASE!!!!
The words “degenerative disk disease” should never pass the lips of a clinician dealing with chronic, axial back pain. When patients hear that they have this, many mold to the expectation that they have a degenerative, diseased, spine and the death-spiral of debility and illness behaviors begin.
IF you choose to use this term, please also start referring to smile-lines as “degenerative face disease” and thinning hair as “chronic fallicular atrophy syndrome”…
“Degenerative face disease”=brilliant!
….unless you have a boat payment due and the patient has great insurance….in that case set them up for a neurosurgeon consult
Exactly!
Thanks for this post, Anthony. I’m sharing with folks. Though so many people do love their diagnoses, don’t they?
Thanks for sharing Kristin. “Yes”, it seems having a diagnosis provides some certainty even if in the end it may be limiting.
Hi there, I have really found this post very useful, and have been trying to search for anything on your site about my condition which has been daignosed along with symptoms as FAI, femero Acetabular impingement.
I am using my ipad and cannot access the search box is covered by the banner at the top!!
Do you have anything on this condition, as I am doing what you say here exactly! Limiting what I do… I have given up my favorite soin classes and swimming. And I am anticipating after prehab ( tho any glute strengthening exercises I am given seem to irritate my hip) to have arthroscopic op to trim femoral head lesion and deal with labral tear… I’m not fully oh fey with the planned procedure. I have been looking a lot online and find passionate folk eg FAI fix… Who advocate a corrective approach vs surgery.
Ypur email today was timely, Tojo I see it was written a year ago.
A pt at my gym introduced me to you about 10 yrs ago and I enjoy your emails and have bought 3 of your DVD …. Which I am guilty of not yet watching! It is all a bit too complex probably… But I am totally fascinated with corrective strategies, tho never easy to apply to oneself!
I have never managed to find a knowledgeable therapist in this sphere, I don’t think we have them in UK?!!
I follow eric cressey, rick kaselj. Mike Robertson, these new FAI fix guys now!! And others
Any advice very welcome , especially if you know anyone here. I see physios, have a good osteopath…
I am a 61 yr old part time dentist, who loves to feel fit… Did jane fiona type exercise in 20’s and 30’s no conditioning or strength training until much later… Had a passion for circuit classes and military fitness…then in 50’s started getting problems! Are you surprised!
Any advice welcome! And your take on FAI
Hi Janet,
FAI is something that seems to be getting more common but is often something that is treatable with postural alignment therapy and many people are able to avoid surgery. When did you first start getting hip symptoms? What were they like? Is it only on one side?
The web and most experts will tell you FAI occurs because your hip bones didn’t form normally in your early years. But I would suggest questioning that. For most people questions like these are relevant: Why was I pain for for many decades and didn’t have any hip problems? It would seem improperly formed hips would cause issues early on. Why is it only on one side? Is it on my dominate leg or weaker leg? Could that be relevant? What causes bone spurs? If I fix the cause of the spurs, it would be logical my body could take the spurs away.
The great thing with postural alignment therapy and exercise therapy is it can be done via Skype from anywhere in the world. I work with clients from all over the world (including the UK) and I know many other therapists do to. Anthony do you?
If you’re wanting assistance understanding if your posture, function, and movement patterns are playing a role in your FAI feel free to contact me for a free posture evaluation or I’m sure Anthony would help you also.
I agree that most patients believe that abnormal findings are the cause of their problems. I also seee first hand that improved mechanics and fitness level tend to reduce discomfort.
You mention studies showing abnormalities and pain, aging and pain and pain without abnormalities. Did you come across any studies showing reduction of pain in patients who engage in exercise and have spinal abnormalities?
Thanks for your contributions to health and pain free movement.
Hi George. There are quite a few studies around the benefits of exercise and pain reduction. The ongoing challenge is which exercise if any is best. Here are two references. I don’t believe they are specific to spinal abnormalities though.
Chou, R., & Huffman, L.H. 2007. Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Annals of Internal Medicine, 147,(7), 492-504.
Exercise is Medicine Australia. 2014. Chronic pain and exercise. http://exerciseismedicine.org.au/wp-content/uploads/2014/05/2014-Chronic-Pain-FULL.pdf.
Anthony,
Great post, very well said! My 18-22 y.o. college students are always shocked when I tell them that if we took an MRI of their spine at least 30% of them would have “abnormal” findings such as disc herniations even though they’re asymptomatic…it’s a wake up call for them not to let imaging dictate their clinical practice as they enter the healthcare and/or fitness professions.
Thanks for adding the great point Jeff. If people of that age understand that reality in their college years, we hope they would be less alarmed at the news as they get older.