This article originally appeared on Ptonthenet.com
Do you own a pair of minimalist shoes? If you do, you’re in good company.
I present and teach all over the world, and I’ve seen minimalist shoe use among my fellow health and fitness professionals increase substantially, especially during the last 3 years. Enter any training facility or health club around the world and you are sure to see personal trainers wearing Vibrams or something similar. In fact, many fitness professionals have done away with other forms of footwear altogether and have embraced minimalist shoes as their full-time footwear.
Minimalist shoes – also sometimes referred to as barefoot shoes – include shoes ranging from traditional-looking shoes with very thin soles and structural support around the rearfoot to tighter fitting “gloves” (like Vibrams) for the feet that allow for separation of each toe. The term “barefoot shoes” is, of course, an oxymoron…a shoe of any kind insulates the skin of the bottom of the foot from coming in direct contact with the support surface, in contrast to going truly barefoot. Still, while much of the relevant research has examined barefoot versus shod running, many have extrapolated the barefoot results to minimalist shoes and used the positive outcomes as a basis to make a shift in their preferred training and day-to-day footwear.
Rather than focusing on the pros and cons of minimalist shoes, this article will instead examine how to maximize the benefits and minimize the risks of going minimalist. Let’s begin by taking a look at the science behind the movement
The Science Behind Barefoot/Minimalist Running & Walking
Many would argue that physical therapist Michael Warburton’s 2001 review of barefoot running in Sports Science was a major catalyst for the minimalist movement’s growth over the last decade. In 2009, journalist Christopher McDougall helped bring the concept of barefoot running to the masses with his bestselling book Born to Run: A Hidden Tribe, Superathletes, and the Greatest Race the World Has Never Seen.
A number of studies have compared the science behind barefoot and shod running (Eskofiera et al., 2011; Altman & Davis, 2011; Hamilla et al., 2011), and of particular interest are the kinetic and kinematic data related to running economy and injury. Daniel Lieberman, professor of human evolutionary biology at Harvard University, has done several studies comparing barefoot and shod running and is often quoted by proponents of barefoot running. One recent study – “Foot Strike and Injury Rates in Endurance Runners: a retrospective study,” published online ahead of print by Medicine and Science in Sports and Exercise (2012) – found that rear foot strikers (typically runners in shoes) had twice as many lower extremity repetitive stress injuries as forefoot strikers (common in minimalist and barefoot runners). The competitive, college-aged cross country runners in the study all wore running shoes. (It should also be noted that this study was partially funded by Vibram USA.)
But does this research on barefoot/minimalist running apply to people who do not necessarily run, yet spend the majority of their time in minimalist shoes?
In terms of walking, lunging, and squatting, etc. the answer is no.
To understand why, we need to first remember that the foot has two basic functional roles for human locomotion:
1) to provide a rigid platform to propel the body forward, and
2) to adapt to the surface it is on as bodyweight is accepted and through mid-stance.
If the surface is consistently hard and flat, the foot will adapt to that surface by consistently flattening out. When running barefoot or minimalist, the forefoot strike creates an immediate need for active myofascial stabilization of the foot and ankle that prevents foot flattening. This does not occur with a heelstrike when barefoot or shod.
But is flattening or pronating the foot a risk factor for injury? Not necessarily. In and of itself, pronation of the foot is supposed to occur. From a functional perspective, what it is important is: 1) how soon after the heel strike pronation occurs, 2) how fast maximal pronation occurs, and 3) how much total pronation occurs. Excessive pronation, however, can be a problem. Overpronation has been shown to correlate with increased tibial stress fractures (Hetsroni et al., 2008) and to affect pelvic alignment (Khamis & Yizhar, 2007). Further, asymmetrical amounts of pronation have been associated with a functional leg length discrepancy (Rothbart, 2006).
Studies show reduced stance times and shortened stride lengths when walking barefoot versus shod. The first peak of ground reaction forces, however, occurs at the same time and with the same shape for both barefoot and shod walking (Sacco, 2010). This means that when walking barefoot (versus running) one does not assume a mid- or forefoot strike. The muscular activity and fascial loading that is so advantageous even on flat, hard surfaces during barefoot/minimalist running is simply not present with barefoot/minimalist walking. As a result, total time and exposure to flat, hard surfaces should be a consideration when you or your clients are wearing a minimalist shoe. A training session on flat, hard surfaces may be beneficial if there is variety in movements and loads the body experiences during that session. Nevertheless, the benefits of wearing minimalist shoes as “everyday” shoes may be debatable for many clients/athletes.
Limitations of Minimalist Shoes
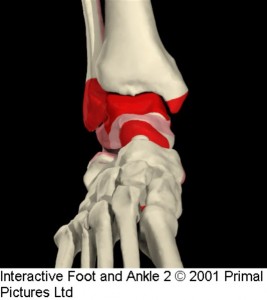
The ligaments and joint capsules of the 33 joints in the foot are rich in proprioceptors, as is the ankle retinaculum. The retinaculum of the ankle has shown to be thickening of the fascia of the foot and leg and are dynamic, non-static structures that are also very rich in proprioceptors (Stecco, 2010). Therefore the plantar fascia of the foot and the ankle are intimately connected. Movement of these joints of the foot and ankle provide valuable information to the central nervous system (CNS) regarding maintenance of our upright posture, weight distribution and locomotion.
When minimalist shoes are worn in highly predictable environments like health club floors, sidewalks, airports, and shopping malls, there is very little variation in the proprioceptive stimulation to the foot. In contrast, environments that have changing surfaces and surfaces of varying density that cause the joints of the foot to move with more variety will likely provide greater proprioceptive input to be processed by CNS. The variety in joint position creates much more diversity of muscular recruitment and fascial loading throughout the myofascial system. The evolutionary development of the human foot without shoes cannot be argued. We have to keep in mind that this development occurred over rocks, roots, branches on grounds with varying inclines in all directions.
A second aspect to acknowledge with the minimalist shoe is the absence of any significant cutaneous stimulation if the shoes are exclusively worn on man-made surfaces. The bottoms of the feet are one of the areas of the body with the highest concentration of cutaneous receptors. These receptors are optimally stimulated when pressures and contact surfaces to the sole of the foot are variable. The fitness floor does not provide this kind of stimulation. For the cutaneuous receptors to be appropriately stimulated in a minimalist shoe, localized and varying pressures would be applied to the foot as with walking on a dirt trail.
The plantar fascia and palmar fascia are tightly connected to the overlying skin. This skin/fascial relationship prevents the degree of sliding between skin and superficial fascia commonly seen in other areas of the body (Benjamin, 2009). This may be another connection in the role touch and pressure play in these two key areas as part of our evolutionary development.
Philip Beach points out in Muscles and Meridians: The Manipulation of Shape (2010) that the soles of the feet are innervated by sensory nerve roots from L4/L5 and S1, and that these spinal segments are the most vulnerable in upright posture. This means we must provide the ample stimulation to the soles of the feet to keep the lower back safe. Beach goes on to call shoes “sensory deprivation chambers that cut down the raw information we need to stand and walk in our precarious upright manner.”
There are other direct links from the sole of the foot to the health of our lower back. The small intrinsic and extrinsic muscles of the foot are innervated from L4 to S3. These same nerves also innervate muscles of the lumbar spine and pelvic floor.
Bringing Minimalist & Barefoot Training to the Fitness Floor
When wearing minimalist shoes themselves or recommending them to clients, trainers should be clear on their benefits and limitations. A body that has always worn supported shoes may not be able to tolerate changes to repetitive loading to the tissues of the foot and/ or lower leg for long periods of time on man-made surfaces. In a traditional training environment, it may be best to introduce the foot to minimalist shoes by reserving them for exercises that always have at least one foot in contact with the floor and involve multi-directional movements that create variability in joint positions throughout the foot and ankle.
It stands to reason that if a minimalist shoe is worn consistently on flat, man-made surfaces, you can use your professional creativity to maximize the potential benefits of stimulating the foot during training sessions through motion and tactile stimulation. This can be done while wearing minimalist shoes, but tactile stimulation is further enhanced when using no foot covering at all.
At the Function First studio, we built a simple but elegant rock garden containing three sections: one with small rocks, one with medium rocks, one with large rocks. Either prior to or at the conclusion of a training session, depending on individual needs, our clients will spend time in their bare feet on the rocks. Some clients walk on the rocks prior to a session to obtain the benefits of mobilizing the plantar fascia and muscles of the foot. Others walk on the rocks at the end of a corrective exercise session to “flood” their feet with cutaneous and proprioceptive input that can be processed and assimilated with the movement strategies facilitated during their corrective exercise program. In either case, there is no way to separate out tissue and joint mobilization from cutaneous stimulation; all happen simultaneously.
A rock garden can be any shape or size as long as the foot fits into it. Ours is made out of plywood and two by fours. The most important aspect of a rock garden is that the rocks are confined and not given the opportunity to slide around very much, if at all.
If the goal is to increase the tactile stimulation to the soles of the feet, we will also use balance pods. The balance pod is dome shaped, about 6 inches in diameter and has raised plastic protrusions. These protrusions provide very specific points of tactile stimulation to any area of the foot in contact with the pod. Clients can stand with each foot on a pod. Because of the dome shape and conforming surface of the pods, the joints of the foot can be taken through movements that are not consistent with flat ground.
Our studio has traditional mat flooring that our clients will exercise on barefoot or in socks. Since the foot is only stimulated through motion on this surface and not through variable pressures or unpredictable foot placement, the rock garden and pods fill that need. Clients are encouraged to spend time barefoot or minimalist outdoors on natural surfaces to stimulate the foot regularly. The same advice applies to anyone with continuous exposure to man-made surfaces.
Liability issues, as well as concerns regarding hygiene and safety, may keep us from going completely barefoot when we want to. As an alternative to going barefoot, minimalist shoes provide an opportunity to appropriately challenge foot function in our bodies’ best interests.
Reviewing the research on barefoot walking versus shod (shoes), we see that the foot strike does not shift to the mid-foot and forefoot the way it does with running. As a result, when seeking the benefits of minimalist or barefoot training, we must be cautious when we extrapolate the impact on walking and everyday use based on running-specific research. The modern adult foot has probably not been exposed to the variable terrain and minimal foot coverings that our ancestors experienced. Removing a client from the support of shoes after decades of wearing them should follow a progressive exposure to surfaces other than those that are flat and man-made. When an environment conducive to foot variability is not present, the fitness professional can minimize the risks and maximize the benefits of the foot by providing an appropriate stimulus such as the rock garden described above.
References
Altman, A. & Davis, I. (2011, May). Comparing Barefoot Running to an Altered Strike Pattern in Shoes. Medicine & Science in Sports & Exercise, 43(5): 59.
Beach, P. (2010). Muscles and Meridians: The Manipulation of Shape. Philadelphia, PA: Churchill Livingstone.
Benjamin, M. J. (2009). The fascia of the limbs and back – a review. Anatomy: 1-18.
Eskofiera, B., Krausb, M., Worobetsa, J., Stefanyshyna, D., Nigga, B. (2011, Feb.) Pattern classification of kinematic and kinetic running data to distinguish gender, shod/barefoot and injury groups with feature ranking. Computer Methods in Biomechanics and Biomedical Engineering.
Hamilla, J., Russella, E., Grubera, A., & Millera, R. (2011). Impact characteristics in shod and barefoot running. Footwear Science, 3(1).
Hetsroni, I., Finestone, A., Milgrom, C., Ben-Sira, D., Nyska, M., Mann, G., Almosnino, S. & Ayalon, M. (2008, January). The Role of Foot Pronation in the Development of Femoral and Tibial Stress Fractures: A Prospective Biomechanical Study. Clinical Journal of Sport Medicine, 18(1): 18-23.
Khamis, S. & Yizhar, Z. (2007). Gait & Posture, 25: 127–134.
Lieberman, D.E., Daoud, A.I., Geissler, G.J., Wang, F., Saretsky, J., Daoud, Y.A. & (2011, Published ahead of print). Foot Strike and Injury Rates in Endurance Runners: A Retrospective Study. Medicine & Science in Sports & Medicine. Retrieved from http://journals.lww.com/acsm-msse/Abstract/publishahead/Foot_Strike_and_Injury_Rates_in_Endurance_Runners_.98750.aspx.
Rothbart, B. (2006, November/December). Journal of the American Podiatric Medical Association, 96(6).
Sacco, I., Akash, P. & Hennig, E.M. (2010, Feb. 3). A comparison of lower limb EMG and ground reaction forces between barefoot and shod gait in participants with diabetic neuropathic and healthy controls. BMC Musculoskeletal Disorders, 11: 24.
Stecco, C., Macchi, V., Porzionato, A., Morra, A., Parenti, A., Stecco, A., Delmas, V. & De Caro, R. (2010). The Ankle Retinacula: Morphological Evidence of the Proprioceptive Role of the Fascial System. Cells, Tissues, Organs, 192(3).
Vincent, K.R., Vincent, H.K., Seay, A.N., Lamb, K.M., Greenberg, S., Conrad, B.P. (2011, May). Effect of Running and Walking in Barefoot and Shod Conditions on Gait Parameters in Trained Runners. Medicine & Science in Sports & Exercise 43(5): 60.
Warburton, M. (2001, Dec.). Barefoot Running. Sport Science.