Originally written for ACE Certified by Kevin Murray
No doctor can write a prescription for creating relationships. They are hard-earned and complex undertakings, particularly with people in pain.
Part of what makes pain so distressing is its lack of predictability. Experiencing pain feeds into a negative reinforcing loop of uncertainty, up-regulating cognitive stressors such as fear, apprehension and anxiety. This often runs parallel with clients’ difficulties in regulating their emotions (Hamilton et al., 2004).
Woven into the fabric of all relationships is the principle of reciprocity. For the health and fitness professional, navigating the arena of pain and relationships requires one to become acquainted with the nervous systems role in analyzing risk and safety.
Neuroception: The Mind’s Mediator
Neuroscientist Stephen Porges coined the phrase neuroception to describe the neural mechanisms involved with subjective perception and evaluation (Van Der Kolk, 2015). Specifically, neuroception helps individuals distinguish whether a situation or individual is safe and trustworthy, or dangerous and distressing.

To the individual experiencing pain, their unique view of the world is interpreted through a nervous system that has an altered perception or risk and safety. Every day situations can become fearful and ambiguous, often resulting in maladaptive appraisals of people who are unknown or unfamiliar.
Experiencing pain has one’s neuroceptive system on overdrive, constantly seeking out potentially threatening stimuli. This state of cognitive hypervigilance makes cultivating relationships exceptionally formidable. To combat such psychosocial stressors, successfully establishing relationships with clients in pain involves understanding the underlying mechanisms which enhance positive neuroception.
This process is governed by innate biological systems that once understood, becomes the inception of all meaningful, heartfelt and trusting relationships.
Mechanisms of the Mind
Have you ever noticed that when someone is genuinely smiling (even if you don’t know them), you find yourself smiling back? What induces this instinctive mimicry? Why do we yawn when we see someone yawning, or wince when someone smacks their shin on a coffee table?
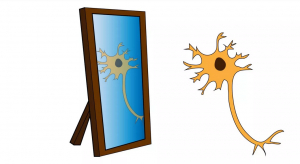
The neurobiological mechanisms responsible for such nonverbal imitation is regulated by highly sophisticated visuomotor neurons referred to as mirror neurons.
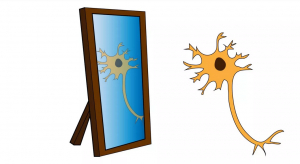
This mirror neuron system (MNS) allows for two individuals, whether lifelong friends or two complete strangers, to simultaneously share neural activity as they attempt to decipher the meaning behind each others nonverbal gestures. The MNS is the gatekeeper of assurance and safety, escorting the manifestation of positive neuroception and is decisively involved in the emergence of all trustworthy relationships. As such, understanding the mirror neuron system’s innate bias towards familiarity and reciprocity becomes a crucial distinction with regards to clients in pain.
For instance, when two people are in-sync and rapport is mutually harmonious, the MNS is fully engaged. People adopt one another’s facial expressions, hand gestures, postures. even acute motor movements without even knowing they’re doing so (Chartrand and van Baaren, 2009). This is known as automatic imitation. Interestingly, being deliberate and purposeful in the mirroring of others nonverbals (intentional imitation) can also facilitate this same mirrored neural activity between two people.
Similar neurobiological functioning ensues via verbal communication. As an illustration, when two individuals and their speech patterns converge, they adopt one another’s vocal qualities such as tone of voice, tempo of speech, even specific words and phrases. Once again, this takes place without any conscious awareness. These neural dynamics lead to mirrored neurological activity between the speaker’s brain and the listener’s brain. This is referred to as neural coupling (Stephens et al., 2010).

In fact, have you ever experienced such high degrees of rapport where you almost knew what someone was going to say right before they said it? This is no fluke. Neural imagining via fMRI technology reveals that when two people are in-sync and engrossed socially, the delay between speech production and the listeners comprehension is so small that one can often anticipate what’s going to be said next (Hasson et al., 2011).
These anticipatory responses suggest as two individuals become acquainted with each others verbal propensities, the more attuned and mirrored their neurological activity is. Neural coupling highlights how verbal imitation can breed a sense of relatedness and commonality, ultimately nurturing the perception of safety and enhancing positive neuroception.
However, when two people are out-of-sync with their nonverbal mannerisms and verbal speech patterns, this brain-to-brain coupling vanishes (Stephans et al, 2010). When incongruencies are present, the perception of safety slowly fades and gives rise to uncertainty. If clients in pain fail to see aspects of themselves in their health and fitness professional, the more likely skepticism has the opportunity to settle in.
In-depth Analysis
The role mirroring plays in socials interactions is ubiquitous. In fact, visuomotor mimicry is so innately hard-wired that one-month-old infants display the mirroring tendencies of smiling, sticking their tongues out and opening their mouths when observing such behavior in others (Lakin et al., 2003).
As two people learn how to navigate the social complexities of interpersonal communication, what are the neurobiological intricacies involved in learning and interpreting the intended meaning of another individual’s linguistics / gestures? Let’s analyze the MNS in-action through a common example:
Spoon Feeding and Neurobiology
As a mother brings a spoon to her infant son’s mouth for the first time, is the child aware of the next sequence required in this exchange? Does the baby open his mouth wide, accommodating for the size and shape of the spoon? Probably not.
Instead, a blank stare of bewilderment is undoubtedly written across the infant’s face. It’s not until the mother visually demonstrates the spoon-to-mouth action that the infant can comprehend what’s being asked of him.
The infants MNS observes their parent demonstrate the action of spoon-to-mouth (intended outcome).
This creates a visuomotor representation and engages the infants own perceptual-motor circuitry.
The infant can then synthesize the visuomotor representation (action-potential) into motor execution, resulting in the reciprocation of the desired task: i.e. successfully transferring food from spoon-to-mouth for ingestion.
Here we witness the MNS and its architecture having the remarkable ability to transform passive observation, into perceptual understanding and then motor execution (Ferrari et al., 2005). Daily social exchanges such as handshakes, waving hello or goodbye, observing laughter or witnessing sadness all involve the MNS and neural coupling effects.
The mirroring of facial expressions can even result in actually adopting the emotions and moods of others (Lakin et al., 2003). This outcome is recognized as empathy, or having the capacity to understand the feelings of others and view the world through their unique perspective.
The interplay between biological and environmental factors requires more sophistication as our social surroundings increase in complexity. This makes congruent communication and mimicry as a medium for cultivating trusting relationships significant, particularly with clients in pain.
So how can you, the health and fitness professional apply these neurobiological insights with your clients in pain to enhance positive neuroception and ultimately establish relationships?
Integrating Neuroscience into Relationship Building
It’s essential to remember what distinguishes the client in pain from general clientele is their altered perception or risk and safety. Never forget, from the moment you meet your client in pain, they’re skeptically evaluating you and how you conduct yourself. As such, taking special care to remove as much uncertainty and unfamiliarity as possible becomes the primary focus. This process begins with the practice of adapting your own verbal and nonverbal mannerisms to match that of your clients.
For example, when communicating verbally, congruency is essential for positive neuroception. Suppose a client begins describing his story of musculoskeletal challenges with soft and gentle vocal qualities. He takes the time to articulate and pauses often. Attempting to mirror and reciprocate these vocal mannerisms follow the neurobiological prerequisites to manifest neural coupling
Should the client also be sitting on the edge of their seat and leaning forward, following suit and mimicking this seated posture engages the visuomotor neurons of their mirror neuron system. Intentionally integrating and reciprocating these verbal and nonverbal idiosyncrasies serves to enhance the possibility of cultivating positive neuroception.

IMAGE TAKEN FROM THE YELLOW BRICK ROAD: A 4-part framework for coaching clients in pain
The matrix of mirroring possibilities includes paying attention to your clients nonverbal features such as facial expressions, eye contact/gaze, body position and proxemics (personal space) and his or her idiosyncratic hand gestures.
Verbal and vocal aspects could encompass specific words or phrases they frequently use, paralinguistic qualities such as tone of voice, rate of speech, vocal modulation and volume, or demonstrating appropriate levels of silence should the client be reserved and introspective. Knowing which aspect(s) to mirror comes down to actively listening and observing the uniqueness of each clients’ communication tendencies.
As clients in pain begin experiencing coherence and familiarity in your communication conduct, their skepticism is superseded with impressions of trust and certainty. Their perception of safety and assurance increases as positive neuroception begins planting its roots.
And while the genesis of cultivating relationships varies from one individual to the next, attempting to enter each client’s world and speak their language helps to nurture the inception of meaningful, heartfelt and trusting relationships with your clients in pain.